Nov 26, 2022 |
PSY 101
|
|
What is the Prevalence of Depression in the United States?
Nov 26, 2022 |
PSY 101
|
|
The COVID-19 pandemic (2020-2021) resulted in significant increases in depression in the United States. However, even with the quieting of the pandemic, depression rates have remained elevated.
National Center for Health Statistics (NCHS) data for 2021-2023
Gallup National Poll, 2025
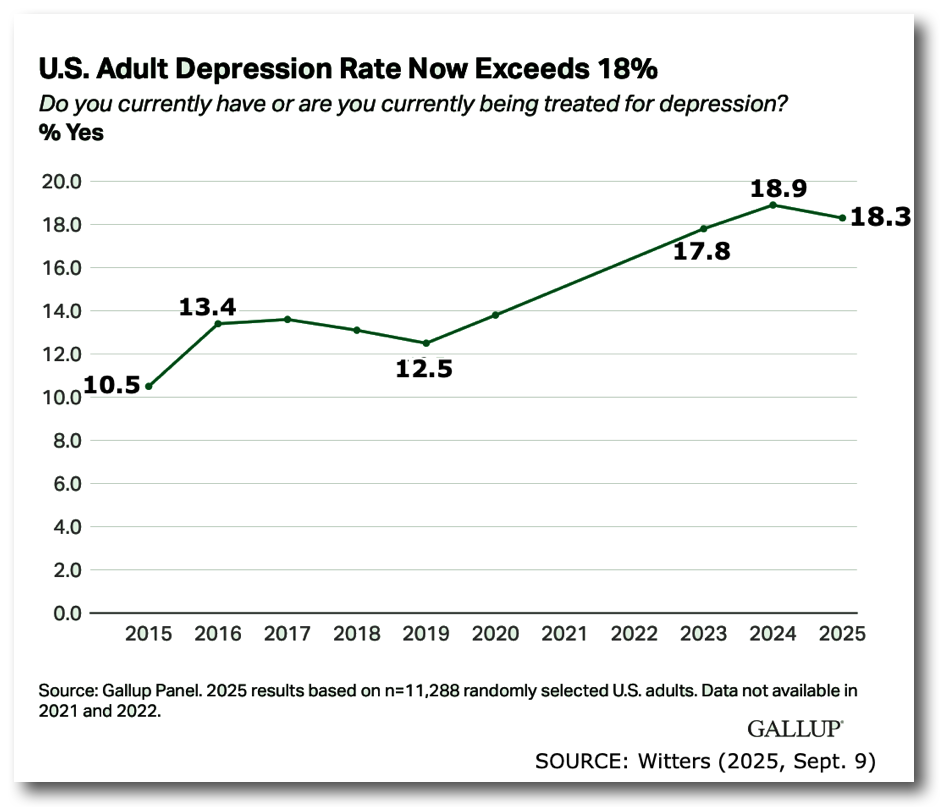
- These data suggest that the level of depression in the United States has continued to grow even after the pandemic
- Women are much more likely to be depressed than men and that difference has been true for over a decade
- The highest rates of depression come in late adolescence and early adulthood and these rates have been growing in the last 10 years
- The highest rates of depression come in poorer families with household incomes under $48,000 a year.
The Dual Face of Mood Disturbance
| Pole I: Depressive Episode |
Pole II: Manic Episode |
|
| Emotional Symptoms |
|
|
| Cognitive Symptoms |
|
|
| Behavioral Symptoms |
|
|
1. Major Depressive Disorder (Unipolar Disorder)
- Marked by the symptoms listed above for a depressive episode
- Note that a unipolar mood disorder marked by a purely manic episode, that is, "pure mania", occurs so infrequently that most psychiatrists/clinical psychologists don't ever see it.
Onset & Course
- At any time, but particularly between 15 and 35 for first episode
- Depressive episodes tend to last for about 5 months
- While the majority of depressive episodes are resolved within 6 months, left untreated most people will re-experience another episode (> 75%).
Prevalence
- NIMH suggests that up to 9.5% of Americans have a depressive disorder in any one year
- Current lifetime risk in the US may be as high as 19% or more (Merikangas et al., 2011)
- THESE RATES WERE TRUE 15 YEARS AGO....NOT NOW.
Some suggestions that, among younger people, the lifetime risk may turn out to be as high as 25-40%
Women are about 2 times more likely to be diagnosed with depression as men.
2. Bipolar Disorder
Note that. beginning with the DSM-5, Bipolar Disorder is treated as a separate disorder from Major Depression.
- Marked by an alternating patterns in which depressive episodes are preceded or followed by manic (or hypomanic or "mild" manic) episodes.
- NEW: In the last five to ten years, some researchers have begun to use a term called "bipolar spectrum disorder" which includes
- the traditional diagnostic category of bipolar disorder ("pure" bipolar disorder = Bipolar I [Depressive & Manic Episodes] and Bipolar II [Depressive & Hypomanic Episodes] disorder), and
- a new category of "subthreshold bipolar disorder", that is, a disorder in which an individual has some but not enough symptoms to actually qualify for a diagnosis of either Bipolar I or Bipolar II Disorders (Merikangas et al, 2007, 2011).
Onset & Course
- Usually develops in late adolescence and early adulthood: vulnerability is highest in the 20s.
- NEW: Often shows a "neuroprogressive" course, i.e., increasing frequency of manic episodes, decreased time between manic episodes, declining overall cognitive performance & functions (Sharma et al., 2016)
Prevalence
- Much less prevalent than depression: for "pure" bipolar disorder the annual prevalence is about 1% and a lifetime prevalence is about 2% (1% for Bipolar-I and 1% for Bipolar-II). However, for the expanded category of "bipolar spectrum disorders, the US rate is about 2.5% annually and about 4% lifetime prevalence. For unknown reasons the US appears to have one of the highest rates of "bipolar spectrum disorder" rates in world (Merikangas et al., 2011)
Gender differences in bipolar disorder are much smaller than in depression. For "pure" bipolar disorder, the rate between women and men is roughly 1:1 (equal). For bipolar spectrum disorder the rate between women and men is about 3:2 (50% greater in women).3. Mood Disorders & Suicide
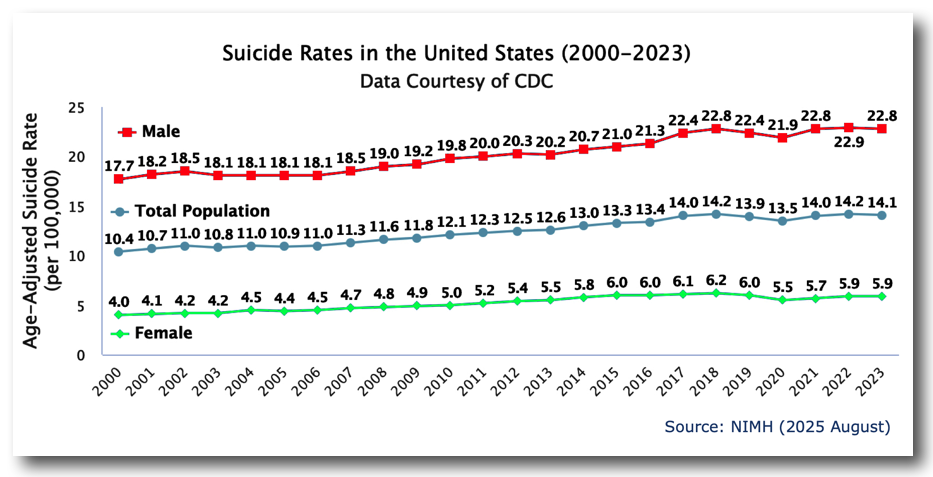
- Suicide rates in the United States increased 37% over the period from 2000 to 2018 and decreased 5% between 2018 and 2020. However, rates returned to their peak in 2022.
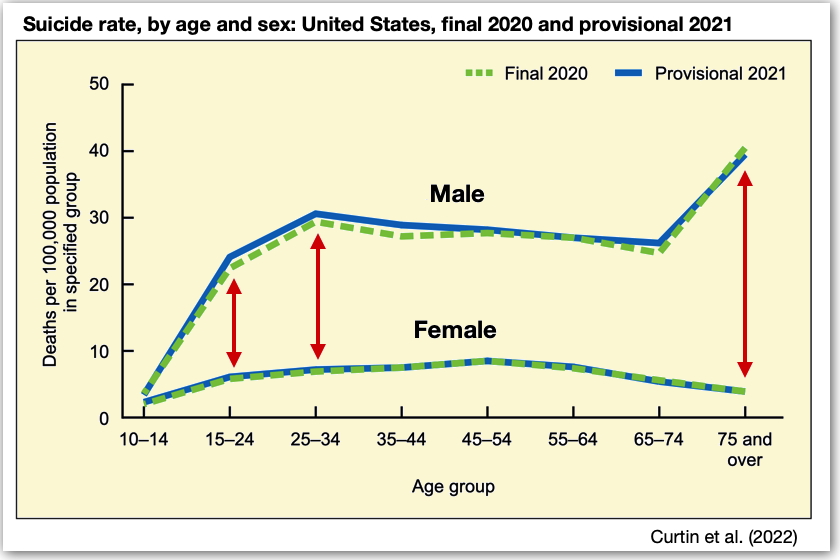
- Suicide in the United States is the 10th leading cause of death overall (48,139 in 2024 provisional), but the 2nd leading cause of death among those aged 10-34 (14,870 in 2023). These numbers are probably an undercount since various "accidents" such as single-driver car crashes may actually be suicide (NIMH, 2025, August).
- The ratio of suicide attempts to completed suicides may be as high as 30 to 1.
- F are 3x more likely than M to attempt suicide, but M are about 4x more likely than F to complete suicide
- 90% of people who commit suicide have some form of psychological disorder, especially among those with depression and bipolar disorder (50-60%).
- Suicide rates are highest among older White males over the age of 75.
- Prediction of suicide is very difficult and inaccurate. The leading indicator tends to be hopelessness.
If you or someone you
know may be considering suicide,
contact
the National Suicide Prevention Lifeline at 988 (English
& Spanish);
Deaf and Hard of Hearing: 1-800-799-4889)
or the Crisis Text Line by texting HOME to 741741.
Etiology (Causes) of Depressive & Bipolar Disorders
Genetic Vulnerabilities
- Strong evidence for genetic vulnerability in depression: Very high levels of concordance for the illness among identical twins (ca. 2/3 or 67%) compared to fraternal twins (15%)
- Bipolar disorder has an even higher genetic vulnerability than unipolar disorder (major depressive disorder). More than 30 specific genetic loci have been found to predispose toward bipolar disorder.
Neurochemical & Neuroanatomical Factors
- Neurotransmitters: Imbalances involving norepinepherine (NE) ↓ and serotonin (5-HT) ↓ are thought to be involved in depressive disorder. Lowered levels of serotonin are particularly related to depression ("the serotonin hypothesis")
- However, the "serotonin hypothesis" is under significant attack as unpersuasive as the primary biological explanation for depression. Newer research suggests that nerve cell death in the hippocampus may be centrally involved in developing a depressive disorder. The mechanism for such death may involve the effects of stress and repeated exposure to corticosteroids (i.e., cortisol; see below). It is notable that long-term antidepressant medications appears to promote new cell growth in the hippocampus.
- We have no generally accepted neurochemical/neuroanatomical theory for the manic phase of bipolar disorder.
Hormonal Factors
Cognitive Factors
- The HPA Axis (hypothalamus-pituitary gland-adrenal gland) releases corticosteroids (= cortisol) into the bloodstream as a reaction to stress.
- Patients with depression often show elevated levels of cortisol.
- Martin Seligman's Two Theories: Earlier theory = Learned Helplessness & later theory = Hopelessness
- Learned Helplessness: People explain setbacks & negative life events using a pessimistic explanatory style, i.e., they attribute the setbacks to causes which are personal (not situational), global, and permanent.
Interpersonal Issues
- Hopelessness Theory proposes that depression is a "final common pathway" in which the effects of a pessimistic explanatory style interact with other factors like high levels of stress, poor self-esteem, etc. to lead to hopelessness which, in turn, leads to depression.
- Evidence?
- Susan Nolen-Hoeksema's 1991 study of depressed persons who ruminate over their situation appear to extend or deepen their depression
- Lauren Alloy et al. (1999): College students were evaluated for negative cognitive style without being actually depressed. Over subsequent 2.5 years, 17% of the "high-risk" students (high negative cognitive style) developed a major depressive disorder compared to only 1% of the "low-risk" students. Further, 39% of "high-risk" students overall had some minor depressive episodes compared to 6% of "low-risk" students.
- There is a significant degree of relationship between poor social skills and depression.
- Qualities like shyness, pessimism, and irritability tend to shut people off from other people who, lacking social support, are more prone to depression.
- Note, too, that individuals with low levels of social support & relationships tend to experience the world as more stressful.
Precipitating Factors: Stress
- Moderately strong degree of correspondence between stress and depression
- Stressors related to depression include (1) childhood maltreatment (i.e., emotional neglect and psychological, physical and sexual abuse) and (2) life events in adulthood (death of a spouse, unemployment, physical or sexual assault, a life-threatening illness, military conscription)
Unipolar Disorder (Major Depression): Two Example Subtypes
- Seasonal Affective Disorder (SAD)
- Annual cycle which brings with it a depressive episode
- In the winter, associated with loss of light in daytime (in Northern Hemisphere)
- In the summer, associated with heat (much rarer) and is particularly noted in areas near the Equator during summer months (e.g., in India)
- Postpartum Depression: Occurs to a mother within a month after the birth of a child (often appearing 2 weeks following birth). More severe than "baby blues" noted below. Mother feels quite down and sad, lack of energy, guilt, hopelessness, inability to feel pleasure and, often, feeling unable to take care of baby. May last for several months or more. Relatively frequently seen, i.e., in about 10% of new mothers.
- "Baby Blues" or "maternity blues" for up to about 2 weeks after birth. Very frequent. Not a "disorder." New mother feels mild anxiety or depression, tearfulness, changeable mood feelings. Probably caused by hormonal changes following birth. In about 50% of new mothers.
- Postpartum Psychosis: A very rare disorder appearing in 1-2 per 1000 births. Woman experiences hallucinations, thought disturbances, and disorganized speech or behavior. It seems to be highly related to an underlying bipolar disorder.
Bipolar Disorder Subtype
- Rapid Cycling Bipolar Disorder: A form of the disorder in which the individual experiences 4 or more manic episodes within one year
Cyclothymic Disorder
- This is a DSM-5 disorder involving alternating periods of elevated (hypomanic) and depressed mood for at least two years in adults (1 year in children/adolescents) without sufficient other symptoms to justify a diagnosis of bipolar disorder
References
Brody, D. J. & Hughes, J. P. (2025, April) Depression prevalence in adolescents and adults: United States, August 2021–August 2023 (NCHS Data Brief No. 527). https://www.cdc.gov/nchs/data/databriefs/db527.pdf
Centers for Disease Control and Prevention (CDC, 2025 March), National Center for Health Statistics. National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are from the final Multiple Cause of Death Files, 2018-2023, and from provisional data for years 2024 and later, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10-provisional.html on Nov 27, 2025
Curtin, S. C., Garnett, M. F., & Ahmad, F. B. (2022, September). Provisional numbers and rates of suicide by month and demographic characteristics: United States, 2021. NVSS Vital Statistics Rapid Release (Report No.24). Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/data/vsrr/vsrr024.pdf
Ettman, C. K., Abdalla, S. M., et al. (2020). Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Network Open, 3(9), e2019686. https://dx.doi.org/10.1001/jamanetworkopen.2020.19686
Ettman, C. K., Cohen, G. H., Abdalla, S. M., et al. (2022) Persistent depressive symptoms during COVID-19: A national, population-representative, longitudinal study of U.S. adults. The Lancet Regional Health - Americas, 5, 100091. https://doi.org/10.1016/j.lana.2021.100091
Merikangas, K. R., et al. (2007). Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry, 64, 543-553. https://doi.org/10.1001/archpsyc.64.5.543
Merikangas, K. R., et al. (2011). Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey initiative. Archives of General Psychiatry, 68(2), 241-251. https://doi.org/10.1001/archgenpsychiatry.2011.12
National Institutes of Mental Health (NIMH) (2025 August) Mental Health Information: Suicide. https://www.nimh.nih.gov/health/statistics/suicide
Santomauro, D. F., Mantilla Herrera, A. M. et al. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398, 1700-1712. https://dx.doi.org/10.1016/S0140-6736(21)02143-7
Sharma, A. N., Fries, G. R., Galvez, J. F., et al (2016). Modeling mania in preclinical settings: A comprehensive review. Progress in Neuro-Pharmacology & Biological Psychiatry, 66, 22-34. https://doi.org/10.1016/j.pnpbp.2015.11.001
Witters, D. (2025, Sept. 9) U.S. depression rate remains historically high. Gallup. https://news.gallup.com/poll/694199/u.s.-depression-rate-remains-historically-high.aspx
This page was originally posted on 11/21/03