Nov 21, 2025 |
PSY 101
|
|
Nov 21, 2025 |
PSY 101
|
|
Psychological Disorders
(Abnormal or Clinical Psychology)
Abnormal Behavior: Is It A Disease?
Demonic Possession
Abnormal behaviordevil's work
- Belief that the "abnormal" individual acts in that manner because of the influence of evil forces (such as the Devil).
"Medical Model"
DSM-5 (2013)
DSM-5-TR (2022)
Abnormal behaviordisease
Modern psychiatry & clinical psychology treats abnormal behavior as a disease.
- Diagnosis: distinguishing one illness from another
- Etiology: the cause & developmental history of the illness
- Prognosis: a forecast or prediction about the probable course of the illness
Problems with the Medical Model
- Labeling with a diagnosis causes social stigma: people feared, rejected, etc.
- This leads to prejudice & discrimination
- Fear of labels may keep people from seeking needed help or treatment
Deficient Problem Solving
Thomas Szasz, MD (died 2012)
Abnormal behaviorsocially unacceptable
- Thomas Szasz, MD: "Abnormal" is a moral judgment about behaviors we don't like.
- Persons who are "abnormal" don't suffer an illness of the mind; illnesses can only be physical
This is very much a minority viewpoint, but does get us to think"Evolutionary Psychiatry" [Wikipedia]
"Darwinian Medicine"
"Madness-as-Strategy" [abnormal behaviorevolutionarily-grounded ways of responding to a challenging world]
- Rather than claiming that all forms of madness or mental disorder are diseases, some forms may actually be proper responses of our minds to a world that is challenging it.
- The "Madness-as-Strategy" model may explain depression, delusions, and other psychiatric symptoms as ways that our minds as designed via evolution can cope with the situations in which it finds itself.
- This is a very new and not widely embraced approach to "mental disorders
Criteria of Abnormal Behavior: What Does "Abnormal" Mean?
Psychology uses the term "abnormal" in at least three different ways:
1. Deviance: The behavior(s) deviates or is different from what society considers to be acceptable.
- Men wearing women's clothing but not the reverse
2. Maladaptive Behavior: There is an impairment in daily life which comes from the behavior(s)
- Behavior interferes with social or personal relationships, work, or ability to take care of oneself, e.g., drug usage
3. Personal Distress: The individual reports significant levels of personal pain or distress
- Depression causes sadness, hopelessness, feeling of doom & gloom.
Note that only a small percentage of people with psychological disorders behave in very strange or bizarre ways.
Psychodiagnosis: The Classification of Disorders
- Prior to 1952, there were no commonly-accepted definitions or descriptions of mental disorders in the United States
- 1952 Publication of the first DSM (Diagnostic and Statistical Manual of Mental Disorders) by the American Psychiatric Association. The DSM provides a description of each type of mental disorder (symptoms, prognosis, associated features, etc.)
Since 1952, there have been a total of eight versions. The latest is the DSM-5-TR, that is, the 5th Edition (Text Revision) published in 2022
DSM-5 defines the general notion of a mental disorder in this way:"A mental disorder is a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities. An expectable or culturally approved response to a common stressor or loss, such as the death of a loved one, is not a mental disorder. Socially deviant behavior (e.g., political, religious, or sexual) and conflicts that are primarily between the individual and society are not mental disorders unless the deviance or conflict results from a dysfunction in the individual, as described above." (American Psychiatric Association, 2013, p. 20)
√ Mental disorders affect our lives negatively
√ Cultural responses to stress and loss like crying or grieving are not mental disorders
√ The fact that a specific culture doesn't like or approve of a person's political, religious, or sexual behavior does not make that behavior evidence of a mental disorder.
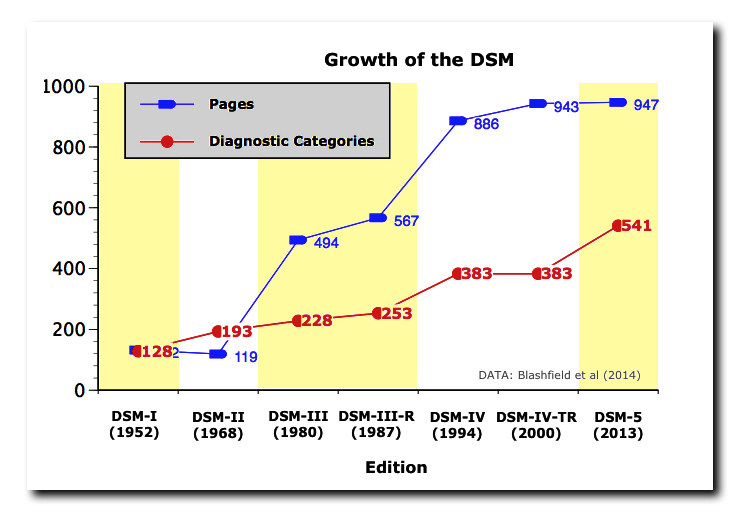
- Over the years there has been a steady increase in the number of diagnostic categories in the DSM (see graph above)
- Some of this has been the result of splitting earlier categories into more focused ones.
- Yet, some critics have claimed that the DSM has created mental disorders out of ordinary life adjustment problems, e.g., caffeine intoxication, tobacco use disorder, disruptive mood dysregulation disorder (multiple temper tantrums in children), etc.
Anxiety Disorders
Central Issue in All Anxiety Disorders
Fear - Apprehension - Anxiety
Four (4) Types in DSM-5
1. Generalized Anxiety Disorder (GAD)
- Chronic high levels of anxiety not tied to a specific threat
- Constant worry
- Physical symptoms such as dizziness, diarrhea, trembling, muscle tension
2. Specific Phobia
- Persistent and irrational fear of a specific object or situation which is not actually dangerous
Some Common Phobias: blood pressure goes up
- Animals = Zoophobia
- Closed spaces = Claustrophobia
- Crossing bridges = Gephyrophobia
- Death or dying = Thantaophobia
- Heights = Acrophobia
- Snakes = Ophidiophobia
- Spiders = Arachnophobia
- Storms = Brontophobia
- Number 13 = Triskaidecaphobia
- Coulrophobia = Fear of clowns
- B-I-I = Blood, Injection, Injury: blood pressure goes down
3. (a) Panic Disorder & (b) Agoraphobia
(a) Sudden & overwhelming feelings of anxiety & fear
(b) Agoraphobia = Fear of going out into public places. While it is listed separately in the DSM-5 and can occur with other types of disorders, it frequently appears in individuals with Panic Disorder
4. Obsessive-Compulsive Disorder (OCD)
- Persistent, uncontrollable intrusions of unwanted thoughts (= obsessions) or urges to engage in useless rituals (= compulsions)
- Obsessions such as fear of harming another or self, failure at work, sexual acts
- Compulsions such as consistent hand washing, checking locks on door, touching objects in a certain order
Etiology (= Causes): Where do Anxiety Disorders come from?
1. Biological
- Moderately high level of concordance in identical twins (ca. 35%) compared to fraternal twins (ca. 15%). This suggests some genetic vulnerability.
- May be related to problems in neural circuits using the neurotransmittter GABA which generally inhibits our nervous system's responses. If it is not working properly, the nervous system may become overly excited and reactive to even small matters.
2. Conditioning & Learning: Fears come from experiences in life
- Some studies have found people can identify specific events which gave rise to the phobia
- Martin Seligman's (1971) Preparedness Theory: some people are biologically (often, genetically) more predisposed to develop fears than others
3. Cognitive Factors
- Some individuals may have a thinking style which promotes anxiety disorders through
- Misinterpreting nonthreatening situations as threatening
- Overemphasizing threat
- Selectively recalling threat information
- Research shows that anxious individual are much more likely to evaluate statements as threatening than non-anxious individuals
4. Stress
- Clearly seen in Post-Traumatic Stress Disorder (PTSD, see below)
- Other types of anxiety disorders often preceded by high levels of stress which, in turn, negatively affect the brain's circuits

Post-traumatic Stress Disorder (PTSD)
- Previously listed in DSM as an Anxiety Disorder, but in DSM-5 moved to a new category: Trauma & Stressor Related Disorders (National Center for PTSD)
- In past wars (e.g, World War I and World War II) soldiers with psychiatric casualities were classified as having "shell shock, soldier's heart, combat fatigue or war neurosis"
- PTSD was originally recognized as a distinctive psychiatric disorder during the early 1970s (Vietnam War).
- For the general adult US population, a lifetime prevalence rate of ~6% (8% among F & 4% among M).
- Among children and teens: 15-43% of girls & 14-43% of boys experience at least 1 trauma. Of those who have had a trauma, 3-15% of girls and 1-6% of boys develop PTSD.
- PTSD is seen most frequently (1/3 to 1/2 of those exposed) in survivors of rape, military combat & captivity, & internment or genocide for ethnic/political reasons (APA, 2013, p. 276).
- The diagnosis requires the following elements:
- Exposure to an event involving danger of or actual death, serious injury, or sexual violence
- War, terrorism, rape, prison stay, assault, domestic abuse, emergency service response work (EMT, firefighter, etc.)
- Via direct exposure, witnessing the trauma or learning that a relative or close friend was exposed to a trauma
- Note that we too often exaggerate what might be a cause of PTSD
- This criterion generally does NOT apply to exposure via electronic media, television, movies, etc. except when the exposure is work related
- Symptoms
- Reliving or re-experiencing the event (memories) in flashbacks, memories, dreams, nightmares, etc.
- Avoidance reactions to trauma related stimuli
- Negative thoughts or feelings that began or worsened after the trauma: emotional numbing, detachment feelings, lack of interest in activities, feeling one has no future, strong negative self-evaluations, inability to remember aspects of the trauma, sense of personal blame
- Arousal and reactivity: concentration difficulties, startle reactions, hypervigilance, irritability & anger, sleep difficulties, dizziness, fainting, heart palpitations
- Duration & Impact: Symptoms have been present for at least 30 days & have caused a significant distress or impairment in social, work, or other important areas of daily life.
- Symptoms of PTSD may appear weeks or months after the traumatic event. Their failure to appear immediately after the event is not an indication against the diagnosis
- If the symptoms are present for less than 30 days, a diagnosis of "Acute Stress Disorder" is made.
References
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders, 5th edition. Arlington, VA: American Psychiatric Association.
Blashfield, R. K., Keeley, J. W., Flanagan, E. H., & Miles, S. R. (2014). The cycle of classification: DSM-I through DSM-5. Annual Review of Clinical Psychology, 10, 25-51. https://dx.doi.org/10.1146/annurev-clinpsy-032813-153639
British Psychological Society [BPS] (2011, June). Responses to the American Psychological Association: DSM-V Development. Retrieved 11/21/2025 from https://dxrevisionwatch.com/wp-content/uploads/2012/02/dsm-5-2011-bps-response.pdf
Durisko, Z., Mulsant, B. H., McKenzie, K., & Andrews, P. W. (2016). Using evolutionary theory to guide mental health research. Canadian Journal of Psychiatry, 61(3), 159-165. https://doi.org/10.1177/0706743716632517
LeBeau, R. T., Glenn, D., Liao, B...and Craske, M. G. (2010). Specific phobia: A review of DSM-IV specific phobia and preliminary recommendations for DSM-V. Depression and Anxiety, 27, 148-167.
PTSD: National Center for PTSD (nd) PTSD and DSM-5. US Dept. of Veterans Affairs. https://www.ptsd.va.gov/professional/treat/essentials/dsm5_ptsd.asp
Seligman, M. E. P. (1971). Phobias and preparedness. Behavior Therapy, 2, 307-321.
This page was originally posted on 11/17/03